Very few plants are as iconic and recognizable as the cannabis plant. This is most likely due to the unique shape of its fan leaves and more than 50 years of international drug policy based upon racial prejudice. Cannabis is one of the oldest medicines used by man, with the first recorded use of cannabis going back more than 3,000 years ago. A genus of flowering plants from the family Cannabaceae, there are three species of cannabis plants: Cannabis sativa, Cannabis indica, and Cannabis ruderalis. Most likely originating in Central Asia some twelve thousand years ago, it is the oldest and first crop cultivated by agriculturists.
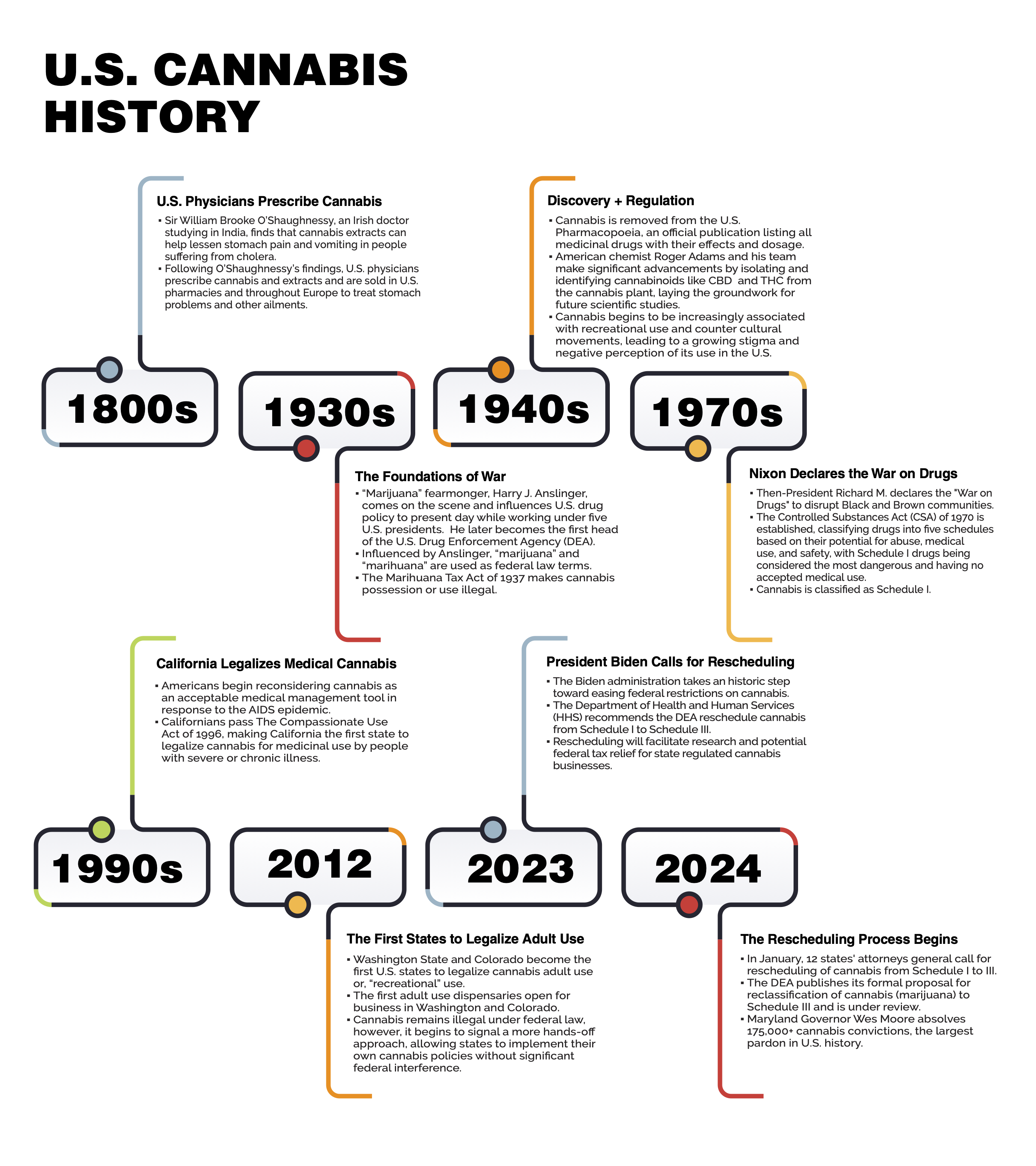
The U.S. cannabis industry is rapidly evolving with significant implications for healthcare, economics, and public policy. The EU and global market follow, in some instances, e.g., Greece and Germany, with federal legalization. Advancements in cannabis science have unveiled its potential therapeutic benefits, leading to a shift in societal perceptions and legislative frameworks. This evolving landscape necessitates a comprehensive understanding of cannabis science, its applications, and the regulatory policies that govern its use. As professionals navigating this complex field, understanding the foundations of cannbis science and policy while staying informed about the latest research findings, market trends, and legal developments are essential to contribute to and capitalize on this emerging industry.
The History of Cannabis as Medicine
Cannabis is one of the oldest medicines used by humankind, with the first recorded use more than 3,000 years ago. A genus of flowering plants from the family Cannabaceae, cannabis sativa, cannabis indica, and cannabis ruderalis, there are three species of cannabis plants, all with uniquely shaped, now iconic, fan leaves. Most likely originating in Central Asia some twelve thousand years ago, it is one of the first crops cultivated by agriculturists for food, medicine, and fiber.
 U.S. State Medical Cannabis Policy + Regulations
U.S. State Medical Cannabis Policy + Regulations
According to a 2024 Pew Research Center report, most Americans now live in a legal cannabis state and have at least one dispensary in their county. Despite this, cannabis remains federally illegal as a Schedule I drug (see diagram), which means that healthcare providers “recommend” medical cannabis versus prescribing medical cannabis. U.S. states have interstate cannabis laws and policies have differences, requiring cannabis industry professionals to have an understanding of how to operate legally and successfully to ensure product quality and safety and navigate the complex landscape of the cannabis industry more effectively.
Optimal state cannabis laws and policies include:
- Product Standards: States set specific standards for the quality, potency, and safety of cannabis products.
- Licensing and Permits: States issue licenses and permits for businesses involved in the cannabis industry.
- Consumer Safety: Regulations often include labeling, packaging, and advertising guidelines to protect patients and consumers.
- Diversity, Equity, and Inclusion Initiatives (DEI): DEI is crucial in cannabis policy to ensure fair access to opportunities and resources within the industry, promote social justice, and address historical inequities in cannabis enforcement and access. Embracing DEI principles fosters a more equitable and sustainable cannabis industry that reflects and serves diverse communities.
Most U.S. state medical cannabis programs require that a patient has a bona fide (legitimate) relationship with the recommending healthcare provider, most often a physician (M.D./D.O.), to ensure responsible use. Several state regulatory bodies require industry employees or “registered agents” to complete a Responsible Vendor Training (“RVT”) program that covers legal requirements, privacy protection, prohibited acts, and statutory and regulatory obligations related to cannabis sales. Licensees are responsible for documenting and preserving training materials and employee attendance records, representing the licensee’s commitment to continuous education and adherence to industry best practices.
Each medical cannabis state’s program has its own website, which provides information on how to become a qualified patient, a list of qualifying conditions, and a link to find state-certified recommending healthcare. Some states allow the regulatory body to be petitioned to add to its respective list of qualifying conditions. Medical cannabis qualifying conditions vary from state to state (see “Managing Diseases and Symptoms”).
As of June 2024, more than 20 states have legalized cannabis for adult use (“recreational) use, allowing adults with a government-issued photo ID to demonstrate they are at least 21. identification to purchase cannabis for personal use without a recommendation from a healthcare provider. For each state’s cannabis laws and regulations, visit The National Conference of State Legislators.
The U.S. Cannabis Industry
There are several key sectors in a regulated cannabis state program market, each playing a vital role in bringing cannabis products from cultivation to consumer while creating a dynamic ecosystem with state laws and policies focused on regulations for patient and adult use consumer safety.
 Cultivators
Cultivators
Cannabis cultivators or growers are responsible for cultivating and caring for cannabis plants. They maintain healthy plants and practice safe, patient-safety feeding methods following state regulations. Growers ensure the plants are protected from pests and microbiols and provided with the proper nutrients for optimal growth.
 Processors
Processors
Processors receive medical cannabis plants from growers and are responsible for refining the essential oils, terpenes, and cannabinoids found in the cannabis owner into safe medical cannabis products and concentrates.
 Dispensaries
Dispensaries
A dispensary is a retail location where medical cannabis patients and adult use consumers purchase cannabis legally and safely. Well-trained dispensaries assist patients in identifying products offering an appropriate dose and recommend a delivery method to achieve optimal results. Best practices are to follow the recommendations of a certified medical cannabis healthcare provider.
 Healthcare Providers
Healthcare Providers
Medical professionals with an active, unrestricted license in good standing with their respective state’s Department of Health who are also actively registered to prescribe controlled substances (e.g., opioids). Because medical cannabis is federally illegal and has been (until very recently) classified as a Schedule I drug, healthcare providers technically do not prescribe medical cannabis; they recommend it. In addition, health insurance providers do not reimburse patients for the cost of any illegal substances.
Each state has regulations restricting which healthcare providers can be certified to recommend providers. These include physicians (M.D./D.O), nurse practitioners, nurse midwives, podiatrists, and dentists.
Patients + Caregivers
 Patients
Patients
Any resident whose registered healthcare provider recommends medical cannabis for a patient to manage a qualifying medical condition. A patient must register with the regulatory agency overseeing the state’s medical cannabis program.
 Caregivers
Caregivers
A caregiver is a person who can purchase medical cannabis from a licensed dispensary on behalf of his or her designated patient(s) and transport the legally obtained medical cannabis to the patient(s).
Cannabis Plant Anatomy
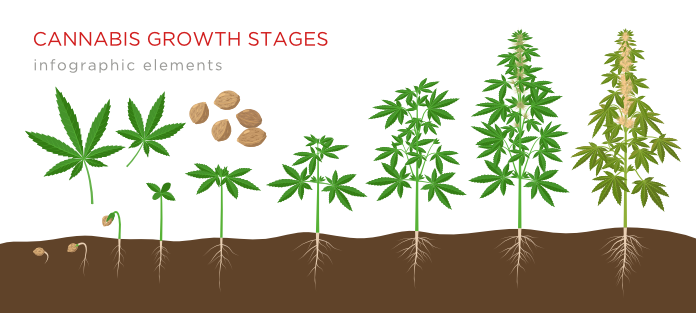
The cannabis plant begins growing like many other flowering species. Cannabis extends up from the ground on thin green stems, incrementally branching from nodes along the way, unfolding unique serrated leaves until the tip of the plant, the cola or bud site, where flowers develop from a protective sheath called a calyx. Cannabis begins to show its complexity in its flower, distinctly different from other common flowering plant species.
Male Cannabis Plants — Male plants do not produce flowering buds but pollen sacs that effectively pop open and allow the wind to spread the pollen to female plants.
Female Cannabis Plants — Female plants grow large flowers known as buds. If pollinated by a male plant, the buds will produce seeds and will not produce potent THC. The cannabis flower is processed into a variety of medical cannabis products sold in medical dispensaries from female plants that have not been pollinated by a male and are able to produce cannabinoids within the flower.
There are three here are three main types of cannabis plants: Cannabis sativa, Cannabis indica, and Cannabis ruderalis. Each type of cannabis plant has its unique characteristics and potential benefits, contributing to the diversity of cannabis products available.
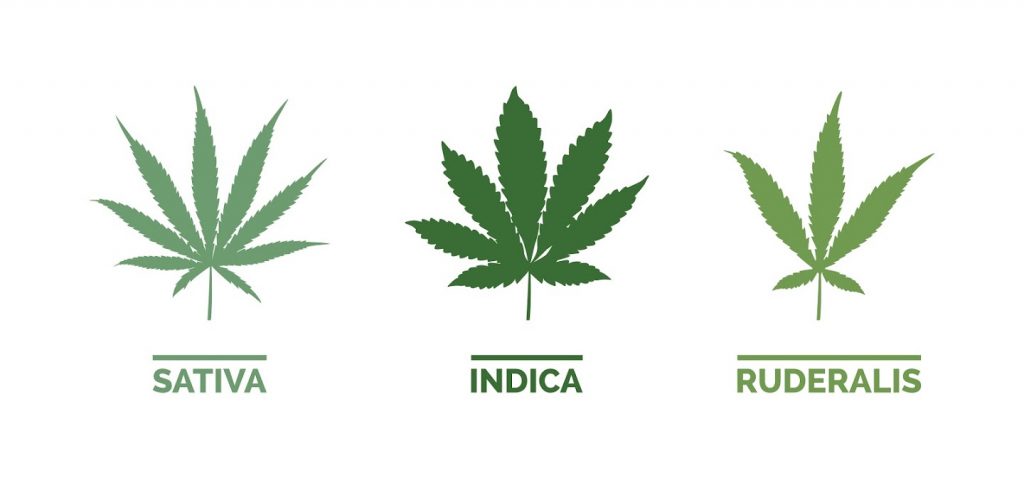
- Cannabis sativa: Sativa plants are typically tall and thin with narrow leaves. They are known for their uplifting and energizing effects, often making them a preferred choice for daytime use. Sativas tend to have higher levels of THC and lower levels of CBD.
- Cannabis indica: Indica plants are shorter and bushier with broader leaves. They are known for their relaxing and sedative effects, which can be helpful for evening use or for managing pain and insomnia. Indica strains generally have higher levels of CBD and moderate levels of THC.
- Cannabis ruderalis: Ruderalis plants are smaller and less common than sativa and indica. They are known for their hardy nature and ability to grow in harsh environments. Ruderalis has lower levels of THC and is often used in crossbreeding with sativa or indica strains to produce hybrids that flower automatically, regardless of light cycles.
Trichomes

Trichomes are mushroom-shaped structures that form on the surface of the cannabis plant, especially when concentrated on the flower (“bud”). They appear as a glistening, sticky layer. While humans prize the cannabis oils and terpenes secreted from these structures, trichomes primarily protect the plant. Within the bulb-like structure of the trichome, the plant changes its cannabinoid profile to adjust for the amount of UV light it receives, acting as a form of sunscreen for the plant. The strong smell and bitter taste of cannabis resins repel herbivores and insects, while antifungals repair chemical damage to the plant.
Terpenes

Terpenes are the aromatic compounds found in the oils of the cannabis plant, along with several plants and flowers. Created by the cannabis plant to attract pollinators for reproductive purposes and detract predators, terpenes are unique oils with several medical benefits. Terpenes interact with cannabinoids such as THC and CBD for medical benefit. This is known as the entourage effect. Terpenes also create medical benefits on their own.
The more common terpenes are identifiable by their intense flavor profile, like citrus, pine, herbs, and black pepper. There are more than 100 terpenes. For more information on individual terpenes and their benefits, visit “terps” on CannabizMD’s Instagram page: @cannabiz_md.
Common Terpenes
Myrcene: This is the most common terpene found in the cannabis plant. It’s a precursor that forms other terpenes, myrcene, which can also be found in mangoes, ylang-ylang, wild thyme, and parsley. This terpene is known for its calming effects, antioxidant properties, and inflammation reduction.
Pinene: This common cannabis terpene has a scent similar to pine needles or Christmas trees. It can also be found in most culinary herbs, like basil, rosemary, and dill. Research has found that it can keep you alert and manage asthma, inflammation, and anxiety.
Caryophyllene: Most spices, like black pepper and chili peppers, commonly contain caryophyllene. Known for its anti-stress properties, it can also be used to manage pain and depression.
Limonene: Often described as a pungent lemon scent, this terpene has stress-relieving qualities. Used primarily as an antidepressant, it can also be used to manage anxiety and inflammation. It also has antibacterial and anti-carcinogenic uses. High concentrations of this terpene are found in lemons.
Linalool: With hints of flowers and freshness, this terpene is known for its calming and anti-anxiety effects. It can also be used to manage symptoms of depression, pain, and insomnia.
Humulene: Also produced in hops and often reminiscent of beer, this terpene is valued medically for its anti-inflammatory properties.
Terpineol: Many oils plants produce contain this terpene, giving it a citrus or floral scent. Used for its anti-carcinogenic effects and especially for sleep, it is known that in high doses, it can have a very sedative effect.
 Naming Conventions for Cannabis
Naming Conventions for Cannabis
The cannabis species names are more valid simply as descriptors of a plant’s phenotype, the observable characteristics of the plant’s leaves, and stature. The terms “strain,” “cultivar,” and “chemovar” are often used in the context of cannabis, but each carries a distinct meaning:
Strain: used colloquially to refer to different varieties of cannabis plants, though this usage is technically incorrect from a botanical perspective. Consumers and retailers commonly use “strain” to distinguish between plants based on perceived effects, flavors, or growth characteristics.
Cultivar: a contraction of “cultivated variety.” It is the correct botanical term for plants that have been selectively bred for desirable traits, such as growth habit, yield, resistance to pests, or cannabinoid content. Each cultivar is given a unique name, often reflecting these traits, its effects, or its origins. In the cannabis industry, the term cultivar should ideally replace “strain” to refer to a specific, cultivated type of cannabis plant, like “Girl Scout Cookies.”
- Chemovar: This term refers to the chemical variety of the plant, classified based on its chemical profile, particularly its cannabinoid and its primary terpene content, which can be analyzed and categorized into groups that share similar chemical profiles (like low THC, high in myrcene and linalool). This classification is important because this chemical composition largely determines the effects of cannabis, and chemovars help in predicting the effects more scientifically than the more ambiguously defined strains or even cultivars.
- Chemotypes classify cannabis plants based on their cannabinoid content, specifically by their predominant cannabinoids like THC and CBD. This system organizes cultivars according to their cannabinoid ratios, dividing them into:
- Type I: THC-dominant plants
- Type II: plants with an equal ratio of THC and CBD
- Type III: CBD-dominant plants
- Type IV: CBG-dominant plants
- Type V: plants (e.g., hemp) with negligible amounts of cannabinoids
In summary, while “strain” is commonly used in casual settings, “cultivar” is the more accurate botanical term for plants bred with specific characteristics, and “chemovar” refers to the classification based on the chemical makeup of the plant. Transitioning to these more precise terms can help healthcare professionals to recommend and patients to find cannabis appropriate for their health conditions.
Cannabis and the Human Body
The Endocannabinoid System (ECS)
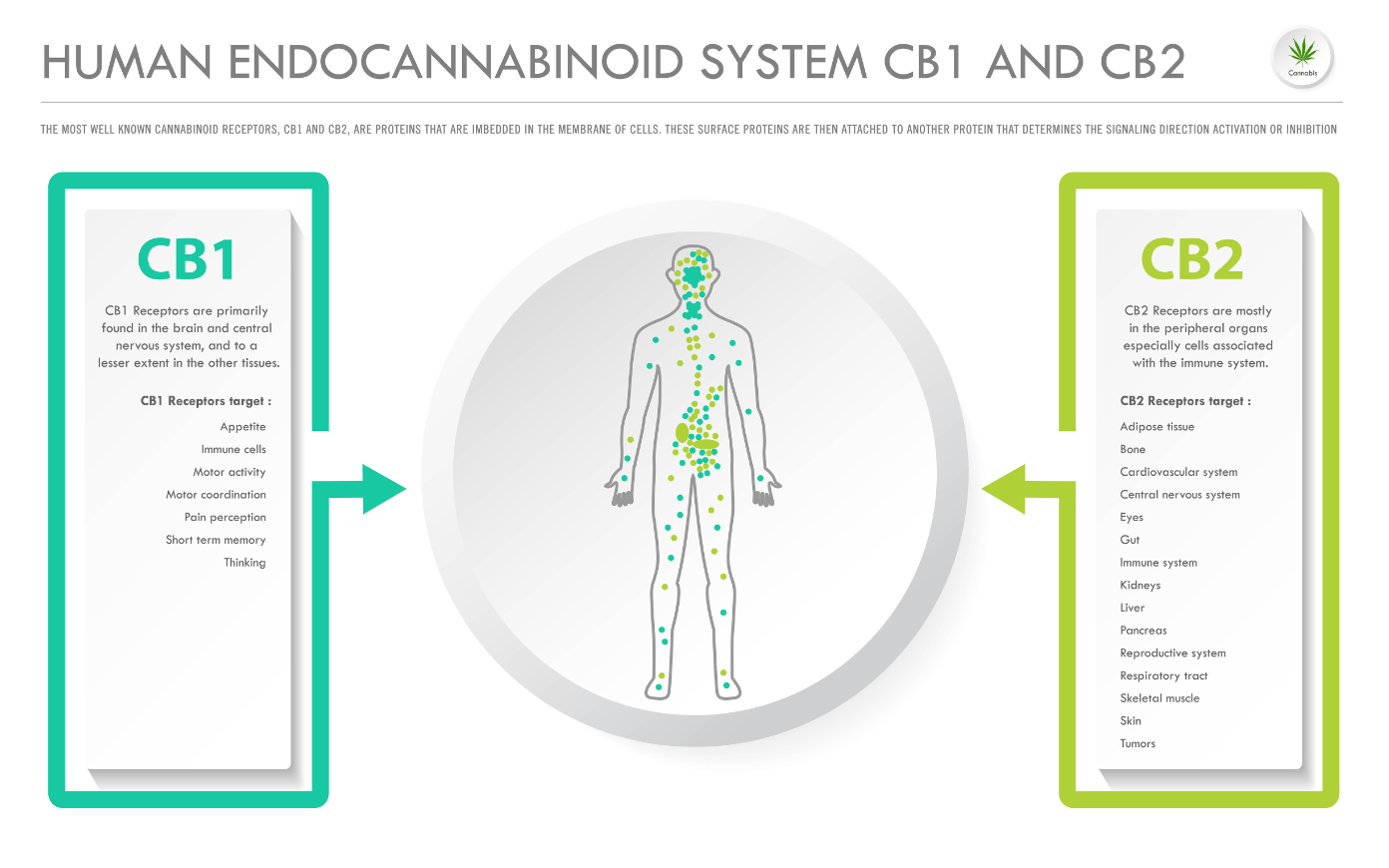
The endocannabinoid system (ECS) is a complex cell-signaling system found in the bodies of all vertebrates, including humans. It is crucial in regulating various physiological and cognitive processes, including mood, appetite, pain sensation, immune response, and memory. The ECS is like the conductor of a complex symphony, regulating other body systems (circulatory, digestive, immune). Here’s a breakdown of its key components and how it relates to the therapeutic use of cannabis:
Components of the ECS
Endocannabinoids: These are naturally produced molecules in the body similar to the compounds found in the cannabis plant. They play a crucial role in the endocannabinoid system, which helps regulate various bodily functions, including mood, pain sensation, appetite, and memory. Two of the most well-known endocannabinoids are anandamide and 2-AG, which bind to cannabinoid receptors to help maintain balance and stability in the body’s internal environment.
Cannabinoid Receptors: There are two main types of receptors:
- CB1 receptors: Primarily found in the brain and central nervous system but also other tissues.
- CB2 receptors: These receptors are mainly located in the peripheral organs, especially cells associated with the immune system.
Phytocannabinoids: These are naturally occurring compounds found in the cannabis plant. They interact with the body’s endocannabinoid system, which helps regulate various functions such as mood, pain, and appetite. Some well-known phytocannabinoids include THC, which is responsible for the plant’s psychoactive effects, and CBD, which is known for its potential therapeutic benefits without causing a high.
- THC: This is the primary psychoactive component of cannabis by binding to CB1 receptors in the brain. THC can also bind to CB2 receptors, influencing the immune system and providing anti-inflammatory effects.
- CBD: Unlike THC, CBD does not bind directly to CB1 or CB2 receptors. Instead, it influences the ECS indirectly, enhancing the level of anandamide and interacting with various receptors in the body, especially the immune system. CBD is known for its potential therapeutic effects, such as reducing anxiety, pain, and inflammation without causing a high. Because it modifies the shape of CB1 receptor, taking CBD along with THC can mitigate some of THC’s unpleasant side effects.
Enzymes: These are responsible for synthesizing and breaking down endocannabinoids and cannabinoids. The most notable enzymes are fatty acid amide hydrolase (FAAH), which breaks down endocannabinoids anandamide, and monoacylglycerol lipase (MAGL), which breaks down 2-AG. This breakdown process ensures that endocannabinoid levels are regulated, preventing overstimulation of cannabinoid receptors and maintaining balance in the body.
There is a growing body of scientific evidence supporting the potential therapeutic uses of cannabis. The most reported applications for medical cannabis are for managing chronic pain and symptoms related to anxiety. Cannabis can also relieve symptoms caused by multiple sclerosis (MS), spasticity, chemotherapy-induced nausea and vomiting, and severe seizure disorders like Dravet and Lennox-Gastaut syndromes.
Discover how cannabis interacts with your body’s receptors in this informative video explaining the CB1 and CB2 receptors work with cannabinoids in the human body: “Cannabinoids and Receptors: A Guide to Receptor Interactions.”
 Potential Therapeutic Uses
Potential Therapeutic Uses
Cannabis may be useful to manage symptoms related to the following diseases:
- Alzheimer’s disease
- Anxiety disorders
- Arthritis
- Asthma
- ADHD
- Autism spectrum Disorders
- Autoimmune Disorders
- Cachexia and Appetite Disorders
- Cancer
- Chronic Fatigue Syndrome
- Diabetes
- Fibromyalgia
- Gastrointestinal Disorders
- Glaucoma
- HIV/AIDS
- Hepatitis C
- Insomnia, Sleep Disorders
- Migraine, Headache
- Multiple Sclerosis and Movement Disorders
- Nausea and Vomiting
- Neuropathy
- Opioid Addiction
- Pain
- Parkinson’s Disease
- PTSD
- Seizure Disorders
- Skin Conditions
- Stress
Routes of Administration and Onset Times

There are a variety of cannabis dosage forms, potencies, and methods (“routes”) of administration, each with a different duration of action. Certain consumption methods are better suited than others for managing disease symptoms. For example, a patient with lung conditions like COPD or emphysema would not be advised to use smoked or vaped cannabis.
Different cannabis delivery methods and their pharmacodynamic effects. The most common delivery methods are:
- Inhalation: Immediate onset (e.g., smoked flower, vaporization).
- Ingestion: Delayed onset, variable effects (20 minutes to 2 hours).
- Liquid Extracts/Tinctures: Moderate onset (20 minutes to 2 hours).
- Cannabis Oils and Concentrates: Variable but often immediate onset.
- Topicals/Bath Soaks: Mostly local effects, variable onset
- Transdermal: Systemic absorption within minutes.
- Suppositories: Local effects; THC does not enter the bloodstream.
 Medical Cannabis Dosing Guidelines
Medical Cannabis Dosing Guidelines
Cannabis pharmacology is notably complex, so effects can vary significantly from person to person. This complexity necessitates careful consideration when determining appropriate dosing. By following dosage guidelines, individuals can better navigate the complexities of cannabis dosing, leading to more effective and personalized therapeutic outcomes.
Here are some recommended strategies to help guide users in finding the right amount to use:
- Start Low and Go Slow: Begin with a low dose and gradually increase it. This approach helps in minimizing the risk of adverse effects and allows the body to adjust to cannabis use. It’s essential to be patient and make small adjustments over time.
- Journal: Keep a detailed record of the cannabis strains (cultivars) used, dosages, and delivery methods. Tracking these details can help you identify what works best for you and elucidate how different environmental factors influence your experience.
- Gradually Adjust Doses and Cannabinoid Ratios: Modulate doses and the ratios of THC to CBD incrementally. The right balance of cannabinoids (including “minor” cannabinoids like CBG, THCV, and CBN) can enhance therapeutic benefits while reducing potential side effects.
- Consult with a Primary Care Physician (PCP): Patients should check with their recommending physician regarding potential drug-drug interactions since cannabis can interact with other medications like the anticoagulant Warfarin and the antiseizure medication clobazam. A healthcare provider can offer personalized advice to ensure safe use.
 Adverse Effects of Cannabis
Adverse Effects of Cannabis
Cannabis should be used carefully and under controlled circumstances. Always consult with a cannabis-educated healthcare provider when using cannabis to manage diseases and their symptoms. Adult use consumers should always share their cannabis use with their primary care provider since it can produce adverse effects and impact the efficacy of pharmaceuticals. The severity and frequency of adverse effects vary depending on the individual, the amount consumed, and the method of consumption.
A variety of cannabis products with higher potency, i.e., higher THC levels, may result in anxiety, paranoia, or delusions. Edibles, in particular, are more prone to causing undesirable outcomes; the patient may not wait for the delayed effect and take more, leading to adverse effects. For this reason alone, it’s critical that the packaging, labeling, and marketing of cannabis comply with state regulations to prevent overconsumption. There is no immediate “cure” for overconsumption; the patient must simply wait for the effects to pass.
Potential Adverse Effects of Cannabis
- Cognitive: Impaired memory, judgment and decision-making
- Physical: Altered blood pressure, heart rate, coordination
- Psychological Effects: anxiety, paranoia
Managing Adverse Effects
Moderation is key when using medical cannabis. Cannabis is unique to every individual; low and high doses can have opposite effects. Unwanted side effects of cannabis can vary in severity from mildly uncomfortable to rare instances that may require medical attention.
Cannabis Use Disorder (CUD)
Cannabis Use Disorder (CUD) is a recognized substance use disorder characterized by chronic and excessive cannabis use, diagnosable only by a healthcare professional. Symptoms include a strong desire to use cannabis despite unsuccessful attempts to quit, significant time spent obtaining and using cannabis, and continued use despite adverse effects on personal and social responsibilities. Additional signs include developing tolerance (needing more cannabis to achieve the same effect or experiencing diminished effects with the same amount), facing withdrawal symptoms, and using cannabis in hazardous situations.
Cannabis Withdrawal
Abrupt discontinuation of cannabis may lead to withdrawal symptoms such as trouble sleeping, anxiety, loss of appetite, headaches, depression, and more. While there are no FDA-approved medications for treating Cannabis Use Disorder (CUD), symptomatic relief is managed on an individual basis and may involve short-term treatments.
Cannabis Hyperemesis Syndrome (CHS)
Cannabinoid Hyperemesis Syndrome (CHS) is a condition resulting from excessive cannabis use, characterized by cyclic nausea and vomiting, and considered a paradoxical effect on the endocannabinoid system. The syndrome is not well understood and often leads to misdiagnosis. Severe cases may require emergency medical attention for dehydration or be life-threatening if not properly managed.
To minimize adverse effects:
- Dispensaries: train attendants to discuss potential negative outcomes with patients when selecting products.
- “Start low, go slow” with dosing.
- Take CBD to offset the effects of THC overconsumption.
- Take a hot shower, which may reduce the unpleasant symptoms. This method is anecdotal, with the theory that the hot water on the skin distracts the CB1 receptors and minimizes the effects of THC and other impairing cannabinoids.
 Protecting Children
Protecting Children
Despite regulations stating that packaging should not be appealing to children, dispensary shelves are filled with products enticing to kids. These exposures have increased calls to poison control centers, emergency department (ED) visits, and hospitalizations. Unintended pediatric consumption can result in hospitalization and expensive diagnostic testing, especially if the caregiver is not forthcoming with the reason for the child’s symptoms for fear of negative repercussions. It is imperative to keep medical cannabis and adult-use cannabis out of reach of children’s access, just as a pharmaceutical product should be.
CannabizMD delivers cannabis science and policy education programs, including workforce development training for Maryland’s cannabis industry funded by a Maryland Department of Labor EARN grant, Responsible Vendor Training, custom programs designed for seasoned professionals entering the cannabis industry, and healthcare provider education. Contact CannabizMD Founder/CEO Jacquie Cohen Roth, MS, for more information.